Pediatric scoliosis
 |
Scoliosis affects 2–3% (61) of children and adolescents, the majority of them young girls. In 80% of cases, the cause remains unknown, and the case is therefore classified as idiopathic. However, scientists are beginning to recognize that the condition may be genetic, which is why it is important the entire family undergo screening when one member is diagnosed. Still in clinical trials and awaiting certification, genetic and blood tests are currently being developed at Montreal's Saint-Justine Hospital and have shown promising results in detecting individuals with an inherited predisposition. The remaining 20% of cases are classified as follows:
|
Progression of Pediatric scoliosis
Idiopathic scoliosis can affect children and adolescents at any stage of development. Here is a brief description of the different types of pediatric scoliosis, as well as a list of indicators to watch for during childhood development.There is unequivocal scientific evidence that demonstrates that the earlier the diagnosis, the more chance there is of preventing the deformity's progression.
Infantile scoliosis
Infantile scoliosis is diagnosed before the age of three. According to the Scoliosis Research Society (SRS), it can be idiopathic (without known cause), or caused by a congenital anomaly of the spine. It can be associated with congenital hip dysplasia, mental retardation or cardiac malformation. This type of curvature often corrects itself.
++++ For infantile and juvenile, when curvature is greater than 20°, Magnetic Resonance Imaging (MRI) is recommended to identify the underlying pathology (syringomyelia, Arnold-Chiari malformation, etc.).
Treating infantile scoliosis can prove to be very delicate and require the joint intervention of several medical professionals.
Juvenile scoliosis
Juvenile idiopathic scoliosis is diagnosed between the ages of four and ten and, according to the SRS, makes up 10 to 15% of all idiopathic scoliosis cases.
++++ As with infantile scoliosis, when curvature is greater than 20°, Magnetic Resonance Imaging (MRI) is recommended to identify the underlying pathology (syringomyelia, Arnold-Chiari malformation, etc.).
Treating juvenile scoliosis is recommended when curvature is greater than 15°. However, in children with a first-degree family history, treatment should be considered even in a mild case.
Adolescent scoliosis
Adolescent idiopathic scoliosis (AIS) appears between the start of puberty and skeletal maturation, and is the most frequent type of scoliosis in this age group. According to the SRS, 30% of cases have a family history of the disease, that is, at least one other family member is also affected. This is why it is so important the entire family undergo systematic screening when one member is diagnosed. Eight in ten of the most severe AIS cases affect young girls.
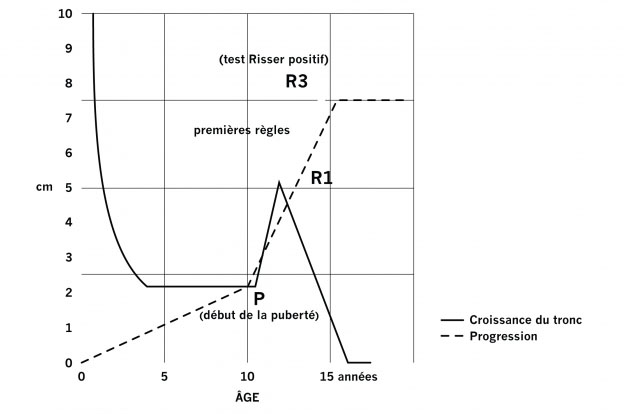
The diagram below, compiled by Duval-Beaupère et al. (27), illustrates the importance of early diagnosis of scoliosis before trunk growth begins to increase. During the adolescent growth spurt, the spine becomes more deformed and as it is submitted to increasing differential pressures that exacerbate the progress of the curvature.
 |
|
The period between the start of puberty until the end of trunk growth remains the most critical stage of adolescent idiopathic scoliosis. |
It is therefore essential to intervene as early as possible in order to control curvature before trunk growth begins increasing, preferably before the age of 12 for girls and 13 for boys.
Treating adolescent scoliosis is recommended when curvature is greater than 15˚. However, in patients with a first-degree family history, treatment should be considered even in a mild case.
Progression indicators according to the SRS (59)
- Measurement of the curvature (Cobb angle)
- Rate of trunk growth versus body growth
- Skeletal maturity at the age of diagnosis, i.e. first signs of puberty
- menstruation for girls
- voice change for boys
- as determined by the Risser sign
- Sex (young girls are more at risk)
- First-degree family history of scoliosis (mother, father, brother, sister)
According to Lonstein & Carlson (44), the younger the age of diagnosis, the higher the progression risk.
Progression risk of juvenile and adolescent idiopathic scoliosis depending on the severity of the curvature according to Lonstein & Carlson.
|
Patient's age of diagnosis |
Cobb angle 5º to 19 º |
Cobb angle 20º to 29º |
|
< 10 |
45% |
100% |
|
11 à 12 |
23% |
61% |
|
13 à 14 |
8% |
37% |
|
> 15 |
4% |
16% |
With scoliosis, the progression risk is at its highest during puberty as during this time trunk growth rate is at its peak. Early diagnosis allows for targetted treatment that may control and possibly reduce curvature as well as minimize the progression risk due to trunk growth.
IN CONCLUSION
 |
Urgent action is needed in cases of scoliosis:
|
To see how the SpineCor® dynamic brace can play an important role in treating AIS and other types of pediatric scoliosis, visit the SPINECOR - PEDIATRIC TREATMENT section.






